Study Finds a Novel Target Molecule to Help Prevent Brain Damage from Hemorrhagic Strokes
With more than 130,000 victims nationwide, strokes are among the leading causes of death in the U.S. each year. According to the Centers for Disease Control (CDC), someone in the United States has a stroke every 40 seconds, with a death every four minutes. But for those who survive, strokes can have a devastating impact, from loss of mobility or speech to severe brain damage.
There are three common types of strokes – transient ischemic attacks (TIAs), ischemic and hemorrhagic strokes. Hemorrhagic strokes account for about 200,000 strokes per year. They are less common than ischemic strokes, but they tend to be more fatal. Of those who survive, about 66 percent suffer some permanent brain damage.
Hemorrhagic strokes result from the sudden rupture of blood vessels in the brain. As blood leaks in the surrounding tissue, it leads to an increased pressure inside the skull, which ultimately leads to brain damage. The brain is very sensitive to bleeding and damage can occur very rapidly.
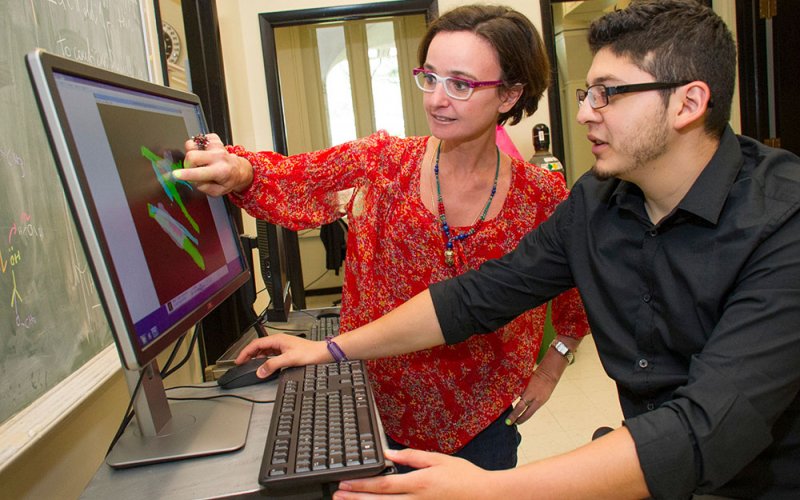
At UAlbany, biophysicist Annalisa Scimemi and her team of researchers are studying the receptors in the brain that may contribute to brain damage immediately after hemorrhagic stroke. If they can understand how the process plays out at the molecular level, they may be able to target certain molecules to limit permanent cognitive impairment and decline following stroke.
According to new research in the March issue of Scientific Reports (a journal of the Nature Publishing Group), Scimemi and her team have just found their answer. The scientists are studying a membrane protein called Protease-Activated Receptor 1 (PAR1), which is commonly found in a particular type of brain cells called astrocytes.
Astrocytes are the most abundant type of non-neuronal cells in the brain. They are intriguing to scientists because they act as midfield players between blood vessels and neurons, being able to interact with both of them. In the hippocampus (a brain region that plays a critical role in memory formation), astrocytes form physical barriers to diffusing chemicals called neurotransmitters, which neurons use to communicate to one another.
“The activation of PAR1 receptors has been suggested to play a key role in hemostasis and inflammation”, said Scimemi, an assistant professor of Biological Sciences at UAlbany and the current President of the Society for Neuroscience Hudson-Berkshire Chapter. “What remains unclear is how PAR1 activation changes the function of astrocytes and neurons.”
In healthy individuals, glutamate release by neurons is key to ensure proper brain function, but the brain needs glutamate only in small amounts and at the right time. A build-up of glutamate in the brain can induce neuronal death. Scimemi and her team showed that, in the mouse hippocampus, PAR1 activation induces rapid structural changes in the fine astrocytic processes surrounding glutamatergic synapses. As a consequence, glutamate is cleared more rapidly from the extracellular space. These changes lead to an impairment of long-term potentiation, the molecular mechanism underlying memory formation.
“These findings are important because they identify PAR1 as a key regulator of glutamatergic transmission in the hippocampus and a possible target molecule to limit cognitive impairment following hemorrhagic stroke,” said Scimemi.
The work was a team effort from UAlbany Biology undergraduate student Amanda Sweeney, graduate students in the Molecular, Cellular, Development and Neural Biology program Kelsey Fleming, John McCauley and Elliot Martin, Computer Science undergraduate Marvin Rodriguez who joined the lab for a summer internship supported by the SUNY Brain Network of Excellence, Dr. Alioscka Sousa (University of São Paulo, Brazil) and Dr. Richard Leapman (National Institute of Biomedical Imaging and Bioengineering, Bethesda, Md.).


