HIV & Hepatitis C: A Complex Web
 |
|
Dean David Holtgrave and associate professor Eli Rosenberg of the School of Public Health. |
ALBANY, N.Y. (May 30, 2019) – Hepatitis C and human immunodeficiency virus (HIV) research out of the School of Public Health is making waves — and national headlines — in the public health community.
Hepatitis C and HIV are distinct diseases with some commonalities. Both are bloodborne viruses with long latency periods in which a person can be infected and transmit it to others without realizing it. Both are more prevalent among people who inject drugs and men who have sex with men.
About 25 percent of those living with HIV also have hepatitis C, according to the Centers for Disease Control and Prevention (CDC), but the presentations of the viruses are entirely different: Hepatitis C affects the liver while HIV destroys immune system cells critical to protecting the body.
How Big is the Hepatitis C Problem?
One of the first steps in addressing an epidemic is getting a handle on how big the problem is, notes Eli Rosenberg, associate professor of Epidemiology and Biostatistics. Rosenberg and colleagues at Emory University and the CDC set out to answer a seemingly straightforward question: What proportion of adults were living with Hepatitis C in each U.S. state?
Because hepatitis C can remain undetected for decades, the question is complex. Published in the American Medical Association's JAMA Network Open, the team found that more than 2 million people were living with the disease in the U.S. between 2013 and 2016. Three-fourths of them were baby boomers, but many areas are experiencing large increases in hepatitis C infection among people under 40 — particularly those who inject drugs.
“Given that recent medical developments have rendered hepatitis C curable, it’s clear that progress needs to be made in both treatment and prevention,” said Rosenberg.
Though the highest numbers are in the western U.S. and Appalachian region, a state-by-state breakdown showed that New York isn’t spared from the epidemic: 750 people out of every 100,000 are living with the infection.
Addressing Hepatitis in New York
In response to the medical breakthroughs rendering hepatitis C curable, government officials across the country are looking for ways to drastically lower the prevalence of the disease — and New York is leading the charge with the nation’s first strategy to eliminate it.
As part of this initiative, Gov. Cuomo created a task force to guide the work and turned to SPH. Dean David Holtgrave is on the 28-member task force, comprised of experts in public health, healthcare, criminal justice and research, while Rosenberg serves on a task force subgroup focused on surveillance, data and metrics.
At the outset of the initiative in late 2018, Rosenberg worked with the Department of Health (DOH) to refine the New York prevalence estimate with additional local information. For example, he developed an estimate specific to inmates housed in correctional facilities — a key setting for higher levels of hepatitis C.
As the task force moves toward making its initial recommendations in June, Rosenberg is helping to develop a framework for the ongoing monitoring of data to track progress toward elimination.
 |
|
Researchers from UAlbany's School of Public Health, Emory University and the CDC found that many areas in the U.S. are experiencing increases in hepatitis C infections among people under 40 - particularly those who inject drugs. |
The Opioid Epidemic: A Ripple Effect
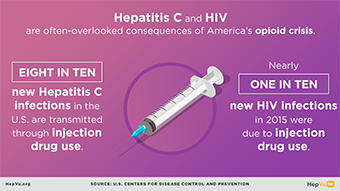
A little-discussed but important complication of the opioid epidemic is that more people are contracting infectious diseases from sharing needles.
“The hepatitis C epidemic is at an interesting junction,” said Rosenberg. “On one hand, we were beginning to see a decline in prevalence because of medical developments. But now, new waves of young people are contracting and transmitting hepatitis C at an alarming rate.”
Funded by Cuomo’s elimination initiative, Rosenberg and Tomoko Udo, an assistant professor of Health Policy, Management and Behavior, are embarking on a project this summer to “look at what’s happening in our backyard,” said Rosenberg. The team will work in three upstate communities — the Capital Region, Plattsburgh and Norwich — to provide hepatitis C/HIV testing to at least 600 people who inject drugs in order to measure the levels of these infections in those hard-hit communities. Additionally, they will study the current risk practices and access to services for treatment and prevention for hepatitis C, HIV and substance use.
“Such information is scarcely available in the state outside of New York City and will be critical to the Department of Health as it tailors its programs to reach the communities experiencing the biggest increases in hepatitis C infections,” said Rosenberg.
Eliminating HIV: An Overly Optimistic Promise?
The elimination of hepatitis C and HIV is on the minds of government leaders beyond the borders of New York. In his 2019 State of the Union Address, President Trump announced a 10-year plan to eliminate HIV in the U.S. Though commendable, this plan needs to be backed by significant funding and resources, said Holtgrave and Rosenberg.
They worked with colleagues at Georgia State University to analyze current HIV surveillance data and developed several national scenarios of care and prevention methods. Their research found that it is possible to reduce new HIV infections by at most 67 percent in the next decade — but only if certain targets are met, such as increasing the percentage of people living with HIV who are sustained in care from roughly 50 percent to over 90 percent. This reduction in infections requires a very large commitment of resources — not just to expand treatment, but also to address barriers to accessing care such as poverty, unstable housing and HIV stigma, Holtgrave said.
“The research shows that an emphasis must be placed on long-term funding — to accomplish a significant reduction in HIV incidence, we must have the adequate resources to develop and sustain a plan for elimination,” said Holtgrave.
The Physical, Mental and Psychosocial Impacts of HIV
A team of faculty from SPH, including Mark Kuniholm, Allison Appleton, Elizabeth Vásquez, Holtgrave and Rosenberg are partnering with SUNY Downstate Medical Center (SUNY Downstate) on a $16 million project funded by the National Institutes of Health to expand the understanding of the physical, mental and psychosocial impacts of HIV. Unlike in the 1980s, HIV infections today can be safely controlled with antiretroviral treatment, but HIV still makes patients more susceptible to chronic conditions and worsens symptoms. The SPH team is comprised of experts in multiple disciplines within public health that will work with the Brooklyn Clinical Research Site at SUNY Downstate on data analytics, cardiovascular disease and aging as they pertain to people living with HIV.
![]() For more news, subscribe to UAlbany's RSS headline feeds
For more news, subscribe to UAlbany's RSS headline feeds
A comprehensive public research university, the University at Albany-SUNY offers more than 120 undergraduate majors and minors and 125 master's, doctoral and graduate certificate programs. UAlbany is a leader among all New York State colleges and universities in such diverse fields as atmospheric and environmental sciences, business, education, public health,health sciences, criminal justice, emergency preparedness, engineering and applied sciences, informatics, public administration, social welfare and sociology, taught by an extensive roster of faculty experts. It also offers expanded academic and research opportunities for students through an affiliation with Albany Law School. With a curriculum enhanced by 600 study-abroad opportunities, UAlbany launches great careers.


