Reducing Opioid Deaths
 |
|
Source: New York State County Opioid Quarterly Reports |
ALBANY, N.Y. (Nov. 28, 2018) – Effective care provided to opioid overdose survivors as they leave the emergency room can make a critical difference in whether the patient gets high immediately or successfully makes it to detox.
Narcan (naloxone) can wear off within an hour and withdrawal is so uncomfortable the patient may seek to use drugs again as soon as possible, said Sandra McGinnis, a senior research scientist at UAlbany’s Center for Human Services Research (CHSR).
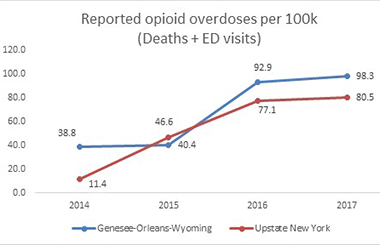
McGinnis is lead investigator on a new CHSR project to conduct an evaluation of the implementation, impact and effectiveness of an opioid prevention program in Genesee, Orleans and Wyoming counties in western New York State.
The CHSR study is aimed at evaluating the follow-up care opioid users receive in three community hospital emergency departments, with the goal of slowing the rate of increase in deaths.
 |
|
Sandra McGinnis |
The Greater Rochester Health Foundation is sponsoring a $115,569 grant to UAlbany’s Center through April 20, 2021, for the evaluation. The Foundation is funding a collaborative program managed by the Genesee/Orleans Council on Alcoholism and Substance Abuse to improve follow-up services for opioid users after overdose or other medical emergency.
The evaluation teams comprises CHSR, the Center for Addictions Research and Albany Medical Center physician and researcher Michael Waxman, M.D., M.P.H. Waxman is an assistant professor of emergency medicine at Albany Medical College and a 2014 School of Public Health alumnus.
Opioid users who are treated by hospital emergency departments are “just the tip of the iceberg,” according to McGinnis.
Many people who overdose on opioids are saved by a family member or friend who administers Narcan (naloxone). They may not go to the hospital at all. In Wyoming County, it is estimated that for every opioid abuser who goes to the hospital for treatment, there are 30 people who do not.
Waxman said the project is “a great example of a comprehensive strategy to reduce the overall burden of opioid use disorder.” He will apply his experience in evaluating emergency department-based preventive intervention in HIV screening and opioid use disorder to the evaluation project.
One of the program aims is to ensure those treated in emergency rooms are connected with a peer/recovery coach, McGinnis said. The project uses the term peer/recovery coach, which encompasses two certified and billable professional titles: certified recovery peer advocate or certified addiction recovery coach.
“In a busy emergency room a physician can’t give one on one support to a patient and their family. If you can have a person there specifically to do that, it is a promising model,” she said.
The idea is to keep the patient sober through withdrawal - ideally until they can get to a medically supervised detox center. The region in the study has few detox facilities, so getting the patient through withdrawal is only one of the barriers to detox.
In addition, more physicians can take training in the effectiveness of using “bridge” prescriptions to ease symptoms. A bridge script for Suboxone, the brand name for buprenophine, can ease withdrawal symptoms.
“That’s what they’re training to do — get people into a structured process of detox and recovery with the help of peer/recovery counselors,” McGinnis said.
Among the goals:
- Slow the death rate from opioid overdose to keep it from increasing more than 25 percent over a three-year period.
- Increase the number trained to administer Narcan by 50 percent.
- Reach 1,800 opioid users per year through a helpline and website for referrals to services and treatment.
Increase the number of opioid patients who are linked with a peer/recovery coach in hospital emergency departments to 90 percent. - Improve Narcan training so that 100 percent of those receiving it are aware of the importance of follow up and providing a ride to services.
“Our role is to collect the data to estimate whether they’ve met the project goals,” McGinnis said. “There are a lot of moving parts and an ambitious agenda.”
Her colleague, Tom LaPorte, a research scientist, will study the effectiveness of care and build relationships with community providers including hospital staff. He will measure fidelity to program standards for the intervention and offer recommendations to improve program implementation.
“We are trying to get at the story underneath the numbers,” he said. “Let’s check the assumptions of the programs. What if there are unanticipated barriers to implementation or what if the intervention has unintended consequences, such as causing peers discomfort? These are the kinds of things that need to be systematically monitored in order to improve,” LaPorte said.
“These types of programs that are aimed to combat something like opioid deaths in the community really require a multidisciplinary approach,” Waxman said. “It can’t just be the physicians, nurses, social workers, and public health workers. It needs to be all these folks working in concert together.”
![]() For more news, subscribe to UAlbany's RSS headline feeds
For more news, subscribe to UAlbany's RSS headline feeds
A comprehensive public research university, the University at Albany-SUNY offers more than 120 undergraduate majors and minors and 125 master's, doctoral and graduate certificate programs. UAlbany is a leader among all New York State colleges and universities in such diverse fields as atmospheric and environmental sciences, business, education, public health,health sciences, criminal justice, emergency preparedness, engineering and applied sciences, informatics, public administration, social welfare and sociology, taught by an extensive roster of faculty experts. It also offers expanded academic and research opportunities for students through an affiliation with Albany Law School. With a curriculum enhanced by 600 study-abroad opportunities, UAlbany launches great careers.


