Identifying Optimal Points of Intervention to Address Racial and Ethnic Disparities in COVID-19 Fatality Rates in New York State

ALBANY, N.Y. (July 1, 2020) – Results from a new COVID-19 epidemiological study have been released from the University at Albany in partnership with the New York State Department of Health (NYSDOH); the findings were published in the peer-reviewed journal, Annals of Epidemiology.
The study aimed to answer three main questions:
- What are the most informative ways to measure fatalities rates across racial and ethnic communities in New York State, and what do these different measures tell us about health disparities?
- Do publicly available data for the state allow for the construction of a COVID-19 outcomes continuum so that population size, rate of SARS-CoV-2 infection, rate of diagnosis of infection, hospitalization and fatality can be meaningfully expressed in one comprehensive figure?
- Can such a continuum be constructed separately for racial and ethnic minority communities in New York and, if so, what lessons can be learned about how to best intervene to address apparent health disparities in fatality rates?
Analyses published in the paper found the following:
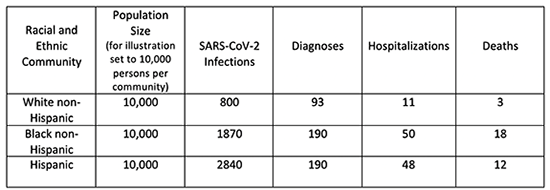
- Estimated per-population COVID-19 fatality rates (deaths divided by population size) were 0.03%, 0.18% and 0.12% for white non-Hispanic, Black non-Hispanic and Hispanic adults. Estimated infection fatality rates (deaths divided by infections in a particular racial or ethnic community) were 0.42%, 0.96% and 0.41% for white non-Hispanic, Black non-Hispanic and Hispanic adults. Estimated case fatality rates (deaths divided by diagnosed cases) were 3.57%, 9.46% and 6.25% for white non-Hispanic, Black non-Hispanic and Hispanic adults.
- The percentage of each population experiencing SARS-CoV-2 infection was 8.0%, 18.7% and 28.4% for white non-Hispanic, Black non-Hispanic and Hispanic adults.
- The percentage of persons experiencing infection who were ultimately hospitalized was 1.4%, 2.7% and 1.7% for white, non-Hispanic, Black non-Hispanic and Hispanic adults.
- The fraction of hospitalized patients who ultimately died was estimated to be 30.2%, 35.8% and 23.9% for white non-Hispanic, Black non-Hispanic and Hispanic adults.
- Examination of these and other disparities across the outcomes continuum by racial and ethnic category suggested that health disparities in fatalities for Hispanic communities relative to white are best explained by differences in infection rates. For non-Hispanic Black adults, relative to white, the disparity in fatalities was primarily driven by differences in both infection-experience and in the need for hospitalization, given infection. (For illustration, see table below.)
- These findings suggest potentially effective points in the continuum to intervention with policies and programs designed to alleviate COVID-19 morbidity and mortality, and the disparities therein; it is especially important to intervene to prevent SARS-CoV-2 infections in the first place, and to do so will require addressing the societal determinants and root causes of these infections.
David Holtgrave, dean of the School of Public Health at University at Albany, said “COVID-19 fatality differences in Latinx and Black communities, relative to white communities, are clear. Our new analysis helps to understand some of the key drivers of these disparities and suggests ways to construct policies and programs to both improve public health and social justice. It is most important to construct policies and programs that address the upstream social determinants of SARS-CoV-2 infection in the first place, rather than wait to intervene near the point of fatality; by then it is too late to prevent and alleviate these disparities.”
For 35 years, UAlbany’s School of Public Health has partnered with NYSDOH on a variety of initiatives, and assisting the Department with the response for a health crisis of the magnitude of the COVID-19 pandemic is a natural fit.
Details on the full study are available at the Annals of Epidemiology website.